You’re Not Alone: Why So Many Parents Face This Question
Hearing that your child might have ADHD can feel overwhelming. You want to do what’s best, but the path forward can seem confusing or rushed. If you’re here, know this: you’re already doing an incredible job by asking questions and seeking understanding.
In our practice, we’ve seen time and again that what looks like ADHD isn’t always what it seems. Sometimes, the real root of a child’s focus, behavior, or emotional challenges lies in how they breathe and sleep at night.
Want to hear more about this connection? Listen to Dr. Kalli’s podcast episode here.
How Sleep-Disordered Breathing (SDB) Can Mimic ADHD Symptoms
When children experience disrupted breathing during sleep (even mild disruption), their brains don’t get the deep rest and oxygen they need. Instead of waking up refreshed, they wake up exhausted—but kids don’t usually show tiredness the way adults do. Instead, they become hyperactive, inattentive, emotional, and impulsive.
Research backs this up. In a study of over 11,000 children, Dr. Karen Bonuck found that children who snored, mouth-breathed, or had disrupted sleep were about 40% more likely to show hyperactivity or inattention by age 4, and almost 60% more likely by age 7 compared to children who slept normally.1
This isn’t just an interesting coincidence—it makes perfect physiological sense.2 When a child’s breathing is even mildly disrupted during sleep repeatedly, they experience:
- Fragmented sleep patterns
- Reduced deep sleep and REM sleep (crucial for memory formation and learning)
- Multiple micro-awakenings throughout the night (often dozens per hour)
- Blood oxygen desaturation
- Decreased oxygen to the brain
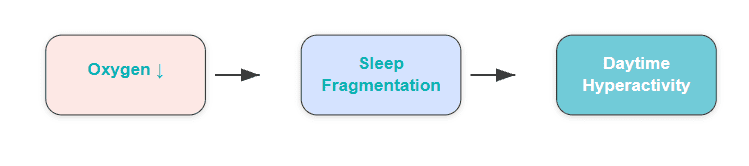
The result? A child who, despite spending a whole night in bed, is effectively sleep-deprived. Unlike adults who may simply become drowsy, sleep-deprived children often become hyperactive, impulsive, inattentive, and irritable—behaviors that are indistinguishable from ADHD.
In our practice, we’ve observed this connection consistently. In fact, every single child who has come to us with an ADHD diagnosis has shown signs of sleep-disordered breathing when properly evaluated.
Signs Your Child’s Behavior Could Be Linked to Sleep Issues
If you’re wondering whether your child’s struggles could be connected to sleep, here are some signs3 we look for:
During Sleep:
- Light or intermittent snoring
- Mouth breathing rather than nasal breathing
- Restless sleep with frequent position changes
- Night sweats (waking with damp pajamas)
- Sleeping in odd positions (e.g., head tilted back and mouth open)
- Teeth grinding (bruxism)
- Pauses in breathing, gasping, or choking sounds
- Sleepwalking or sleep-talking
In our own family, we’ve seen these symptoms firsthand. We regularly found our daughter in different positions in her crib and drenched in sweat after naps—classic signs of sleep-disordered breathing that we recognized and addressed early.
During the Day:
- Daytime sleepiness or paradoxical hyperactivity
- Morning headaches
- Dark circles under the eyes
- Difficulty concentrating
- Irritability or mood swings
- Trouble waking up in the morning
- Behavioral issues at school
- Poor academic performance despite normal intelligence
These signs are not a diagnosis on their own, but they are important clues worth exploring.
Why ADHD Diagnosis Often Misses the Root Cause
When a child shows signs of ADHD, the conventional approach often moves quickly toward:
- Behavioral assessments
- Medications (stimulants or antidepressants)
- Behavioral therapy
- Academic accommodations
While these strategies can be critical for many children, they are often designed to manage symptoms—not investigate potential root causes.
We often see children prescribed powerful medications, like stimulants or antidepressants, without a comprehensive evaluation of their sleep and breathing. This isn’t because providers don’t care—it’s because the connection between sleep-disordered breathing is still under-recognized in many standard medical pathways.
As airway-focused providers, we’re trained to look for these patterns, and when we do, we often find contributing factors that have gone unnoticed. Medications can be life-changing for some children, but they also come with serious considerations—including effects on growth, sleep patterns, emotional regulation, and long-term brain development.4
In our practice, we take a root-cause-first approach. Before a patient considers medication, we recommend seeking out the following from an established practitioner of airway dentistry:
- Comprehensive airway assessments
- Sleep quality evaluations (often including a home sleep study or in-lab study)
- Early treatment of airway restrictions (using airway-expanding dental appliances, myofunctional therapy, or referrals to ENT specialists)
- Ongoing monitoring and adjustment as a child grows
Many parents are shocked to discover just how frequently their child’s breathing is disrupted during sleep, and this doesn’t mean you’ve failed your child—there just may be a missing piece that deserves a closer look.
There may be more to their ADHD diagnosis.
Start with a sleep and airway evaluation to rule out root causes.
What a Sleep and Airway Evaluation Looks Like at The Airway Dentists
Our airway evaluations are gentle and simple, but thorough—the process will help rule out any root causes of ADHD symptoms that are linked to sleep and breathing. If we find symptoms linked to sleep and breathing, we have tools that often resolve them.
Here’s what you can expect:
- Sleep & Health Questionnaire: Before your visit, we’ll ask you to complete a detailed form about your child’s sleep habits, behavior, and health history.
- Digital Scan (iTero): A 3D scan captures your child’s bite and oral structures, helping us assess space and development.
- Intraoral Exam: Our dentists will examine the tonsils, tongue posture and function, bite and jaw development, and the soft palate—looking for signs of restriction or underdevelopment. Issues like a narrow or vaulted palate, enlarged tonsils, or restricted tongue movement can all contribute to disrupted sleep.
- Sleep Study (if needed): We may send you home with a sleep ring—a small device your child wears for 2 nights. Their sleep data is collected through your phone and later reviewed by a board-certified sleep physician—who will determine if/how often your child’s breathing is disrupted overnight.
Understanding your child’s “sleep architecture”—their cycles of deep sleep, REM sleep, and light sleep—is crucial because disruptions can profoundly impact memory, learning, and emotional regulation.
- Diagnosis & Treatment Plan: We’ll go over the results of the entire evaluation with you and discuss next steps. If treatment is recommended, we may take a CBCT scan (3D xray) and clinical photos at that time.
Real Results: When Treating SDB Improves ADHD Symptoms
When we identify sleep-disordered breathing early, the results can be life-changing.
One young patient, an 11-year-old boy, came to us after years of academic struggles and behavioral challenges. A sleep study revealed his breathing stopped 16 times per hour—a severe level of sleep apnea for a child. After a combination of airway expansion therapy treatments, his health, focus, and mood dramatically improved.
Stories like his aren’t rare in our practice. They show what’s possible when we look beyond labels and address the root cause.
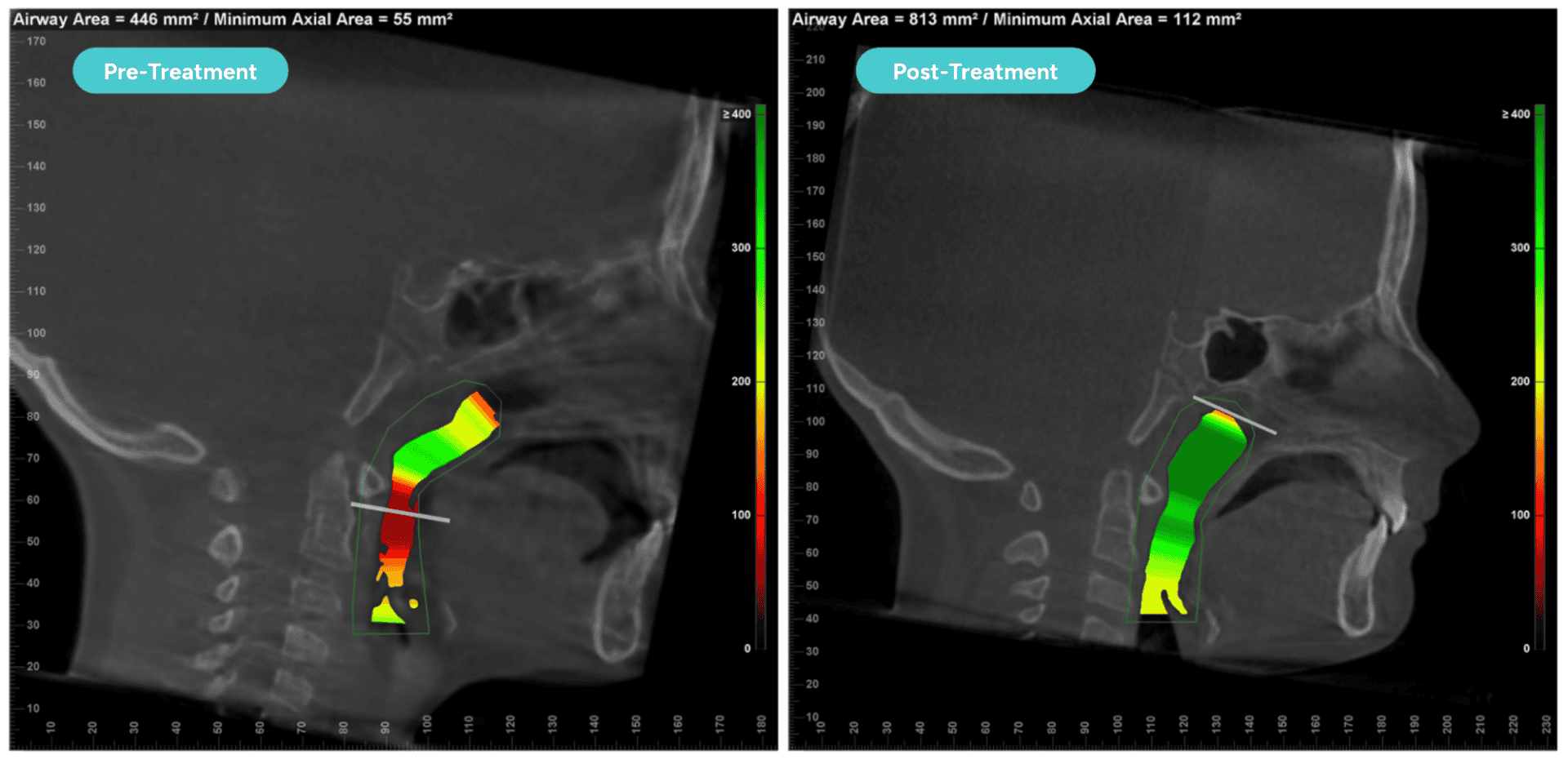
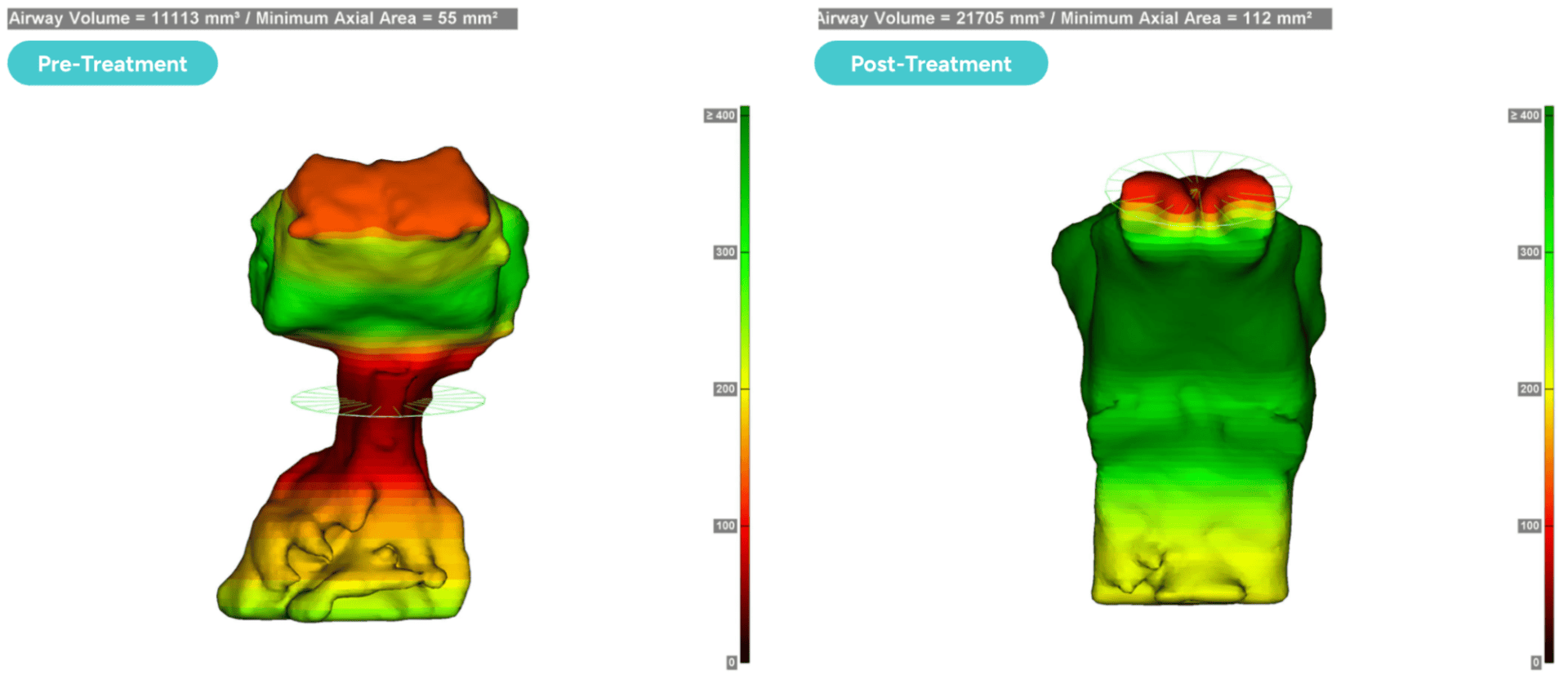
The images below come from another patient who saw a reversal in ADHD symptoms—illustrating the noticeable difference in how the airway functions pre- and post-treatment. When we treat the airway itself and make more space for better breathing, we can see dramatic changes in both structure and function. Improved breathing supports deeper sleep—deeper sleep supports focus, learning, and emotional regulation.
Why Early Intervention Matters
One of the biggest misconceptions in orthodontics and pediatric care is that we should “wait until all the permanent teeth are in” to address jaw and airway issues. But by ages 12–13, boys are about 90% developed in their head and neck structure, and girls are about 94% developed.5 This rapid development timeline is one reason why early airway evaluation is so important. Research has shown that underdeveloped airways can contribute to behavioral and cognitive challenges in children.6
Early intervention, starting as young as age 5–7, allows us to:
- Guide jaw growth to support healthy breathing
- Create space for proper tongue posture
- Encourage nasal breathing habits
The earlier we act, the easier treatment becomes and the better the outcomes we can achieve.
Furthermore, the American Association of Orthodontists recommends kids be examined for orthodontic treatment by age 7.7
What to Do If You’re Facing an ADHD Diagnosis
Receiving a diagnosis can feel urgent—but it’s ok to take a step back and explore what else might be contributing. If your provider has diagnosed your child with ADHD, here are steps you should take:
- Request a sleep evaluation. Advocate for a sleep study before starting medication.
- Observe and record sleep behaviors. Watch for mouth breathing, snoring, sweating, or restless sleep.
- Seek an airway-focused dental evaluation. Not all providers are trained in airway assessments, so seek out one who is.
- Ask about comprehensive treatment approaches. Medications may help manage symptoms, but addressing sleep and breathing may reveal the root of the problem.
- Get second opinions if needed. It’s okay to ask more questions and explore different perspectives.
Remember: gathering more information doesn’t delay help—it strengthens it.
Think your child’s ADHD symptoms might be connected to sleep?
An airway evaluation can uncover what’s really going on.
Sources:
- Bonuck, K., et al. Sleep-disordered breathing in a population-based cohort: behavioral outcomes at 4 and 7 years. Pediatrics, 2012.
- Pediatric Obstructive Sleep Apnea. Mayo Clinic, 2022.
- Sleep Disorders in Children. Sleep Education, 2023.
- Sleep interventions for children with attention deficit hyperactivity disorder (ADHD): A systematic literature review. Sleep Medicine, 2023.
- The Craniofacial Growth Consortium Study, cf. https://pmc.ncbi.nlm.nih.gov/articles/PMC8577187/
- The Link between Pediatric Obstructive Sleep Apnea (OSA) and Attention Deficit Hyperactivity Disorder (ADHD). Children (Basel), 2021.
- https://aaoinfo.org/blog/when-should-my-child-see-an-orthodontist-age-7/