Understanding the Real Cause of Bedwetting
When Bedwetting Isn’t Just a Bladder Problem
Bedwetting—also known as nocturnal enuresis—affects many children beyond the toddler years. If your child wakes up in wet sheets night after night, the hardest part isn’t the laundry—it’s watching their confidence shrink. I’ve been there, 2 a.m. pajama changes and all, wondering what we were missing.
As a functional dentist who looks at the whole picture—especially how kids breathe during sleep—I’ve learned that bedwetting is often a symptom, not the real issue. And when we treat the root cause, kids can stop wetting the bed without relying on alarms, schedules, or meds.
Worried that breathing might be the missing piece?
If your child shows several of these signs, we’d love to help.
At The Airway Dentist, we specialize in identifying sleep and airway issues that often go unnoticed – but make a huge difference. Contact one of our Houston or Austin area offices to learn more about your options
What Bedwetting Has to Do with Breathing (Yes, Really)
Bedwetting is more than just a potty training hurdle. It’s tied to how a child sleeps and breathes. Research and our own experience show a strong connection between sleep-disordered breathing (like mild sleep apnea or mouth breathing at night) and bedwetting in kids.
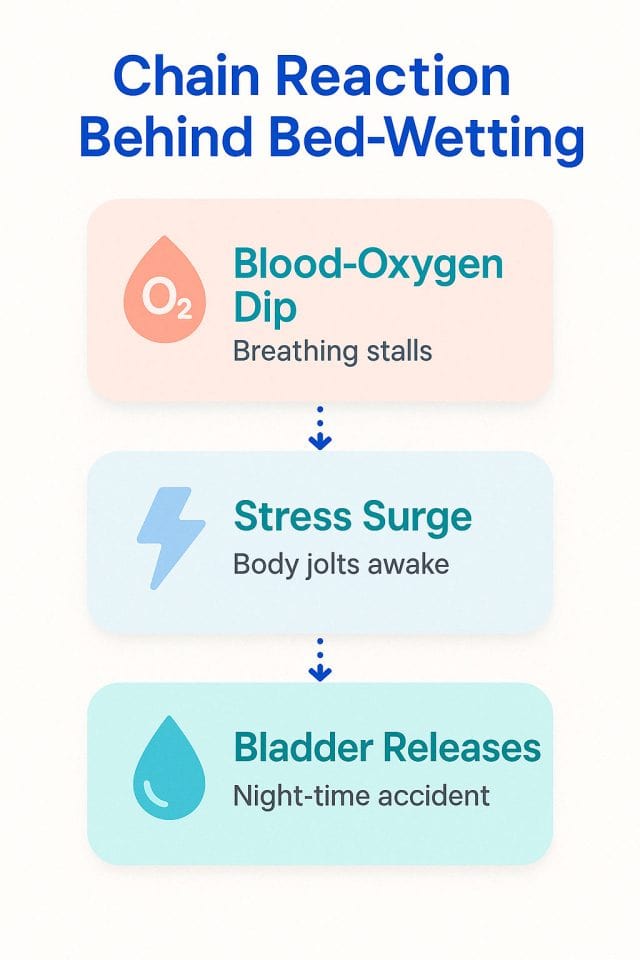
Here’s what happens:
- A child has a breathing disruption while asleep
- Oxygen levels drop
- The brain sounds the alarm: time to go into emergency mode
- Oxygen-rich blood flow shifts to protect vital organs
- Less oxygen reaches the bladder, which can trigger it to release
In short, the body prioritizessurvival over bladder control. And this can happen night after night.
What Happens When We Treat the Real Cause
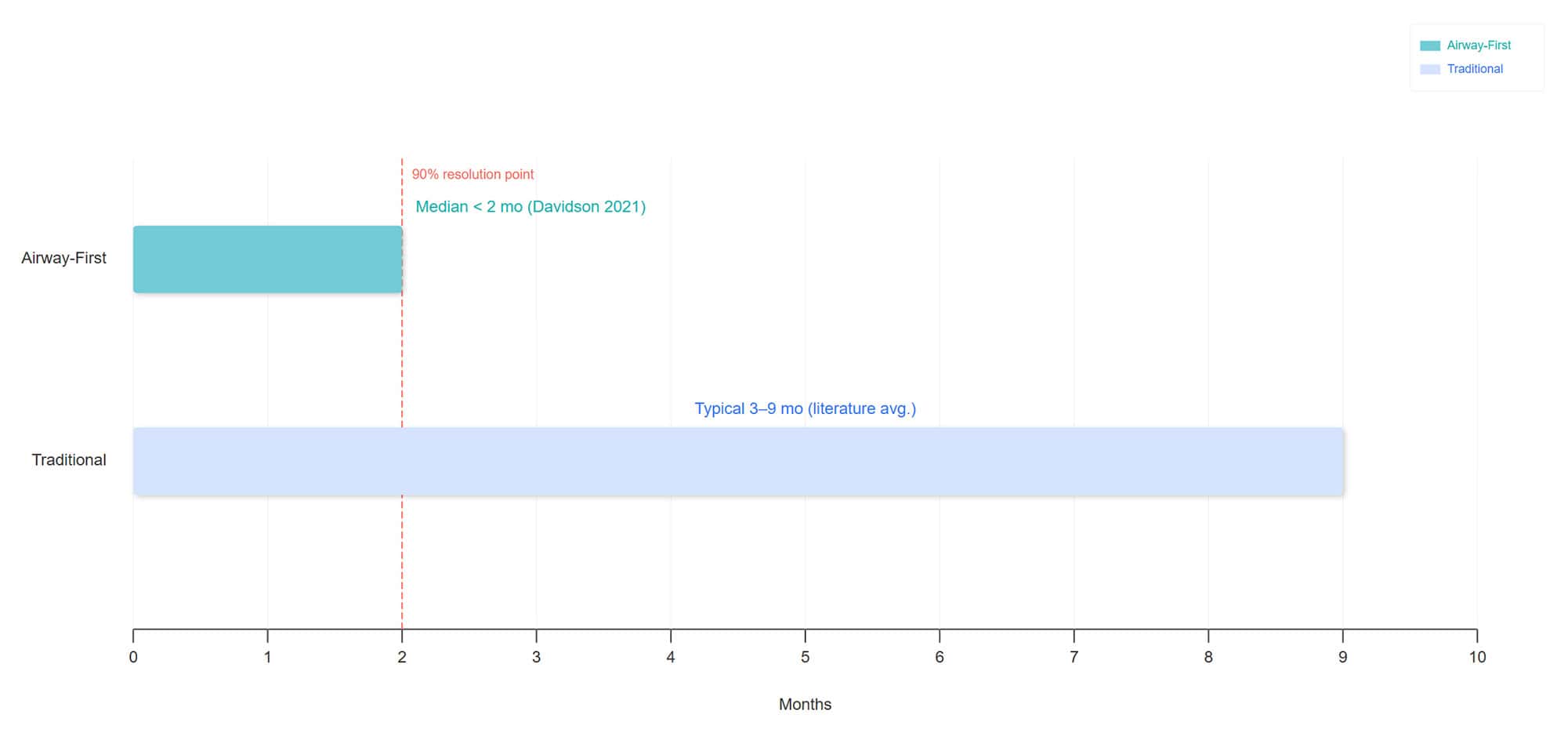
A study published in The Journal of Sleep Disorders and Therapy followed 37 kids (average age: 7½ ) with both bedwetting and sleep-disordered breathing. After airway treatment (the kind we use at The Airway Dentists), 87% stopped wetting the bed entirely. Another 10% saw big improvements. Only one child didn’t respond. And the best part? Results came fast. Most kids were dry within two months—much quicker than traditional approaches, which can take years (if they work at all). These results are consistent with what we see with our own patients.
How Quickly Bedwetting Improves: Airway-First vs. Traditional Treatments
Signs That Sleep May Be the Missing Piece
Clues Your Child’s Bedwetting Might Be a Sleep Issue
Bedwetting rarely happens on its own when sleep-disordered breathing—like sleep apnea or mouth breathing—is part of the picture. If your child is wetting the bed, look for these additional signs that breathing disruptions during sleep may be the real issue:
While your child sleeps:
- Snoring (even lightly)
- Mouth breathing
- Tossing and turning
- Night sweats
- Sleeping in odd positions (like head tilted back or on knees)
- Teeth grinding
- Gasping, choking, or pauses in breathing
During the day:
- Tired even after a full night’s sleep
- Dark circles under the eyes
- Trouble focusing or sitting still
- Mood swings or behavior challenges
- Frequent sore throats, ear infections, or congestion
I noticed these signs in my own daughter before we addressed her airway—sweaty naps, mouth breathing, restless sleep. Once we had her tonsils and adenoids removed, her sleep (and mood) improved dramatically.
Could This Be What’s Behind Your Child’s Bedwetting?
If your child is still struggling with bedwetting despite trying the usual fixes, you’re not alone. Many parents overlook the role sleep and breathing might be playing. These simple questions can help you figure out if it’s time to look deeper:
- Does your child snore or mouth-breathe at night?
- Are they hard to wake or seem unusually deep sleepers?
- Do they still seem tired in the morning?
- Do they grind their teeth in their sleep?
- Have you tried the usual tricks—alarms, meds, fluid limits—with little success?
- Does your child have allergies, frequent congestion, or chronic sniffles?
If you’re nodding “yes” to several, it might be time to explore the airway-bedwetting connection.
Traditional Fixes vs. Root-Cause Solutions
Many families try everything—alarms, fluid limits, medications—only to feel discouraged when bedwetting continues. These traditional approaches can help manage symptoms, but they often miss the root cause: what’s happening during sleep.
When children struggle with disrupted breathing at night, like mouth breathing or sleep apnea, it can interfere with their body’s ability to control the bladder. That’s why so many of the usual tools fall short. The real solution often lies not in the bladder, but in the airway.
Why the Old Advice Often Falls Short
Traditional treatments can offer short-term relief but don’t address what’s triggering the body to lose bladder control in the first place: stress responses caused by low oxygen during sleep.
A study in The Journal of Pediatrics found that nearly half of children with even mild sleep apnea wet the bed—almost three times more than kids who breathe normally. That’s a strong link between disrupted sleep and bedwetting.
Conventional treatments often:
- Provide only temporary relief
- Work inconsistently
- Take a long time to show progress
- Add stress for kids and parents
- Fail to create lasting results
On top of that, there’s still a stigma around bedwetting. Many parents feel shame or fear it’s a behavioral issue, when in reality, it may be a physical sleep-related condition. UK guidelines note that even when medications appear to work, about half of children start wetting again within 12 weeks of stopping.
A New Approach: Solving the Problem at the Source
When we shift our focus from managing symptoms to addressing what’s happening during sleep, we see real results. Treating airway issues—like enlarged tonsils, mouth breathing, or narrow palates—can dramatically improve not only bedwetting, but also mood, behavior, and daytime focus.
Children who receive airway-focused care often stop wetting the bed within weeks. They sleep more soundly, breathe better, and wake up more confident—not just dry. It’s a whole-child approach that supports healthier growth and development long-term.
The Unexpected Wins When Breathing Gets Better
When sleep improves, kids thrive. We’ve seen children who were tired, cranky, and soaking wet every night transform into confident, well-rested humans after airway-focused treatment.
Other benefits can include:
- Better sleep quality
- More energy and focus
- Fewer meltdowns or mood swings
- Healthier jaw and facial growth
- Lower risk of adult sleep apnea
- Fewer colds and ear infections
Dry nights are just the start.
Taking the Next Step
What to Do if You Suspect Sleep Is the Issue
If you’ve checked all the traditional-fix boxes, yet bedwetting persists, it might be time to look in a different direction. Here’s how to start exploring whether sleep and breathing might be the missing piece:
- Watch your child sleep – Look for signs like mouth breathing, snoring, restless movement, sweating, or unusual sleep positions.
- Track daytime behavior – Fatigue, irritability, trouble concentrating, or chronic congestion may point to poor-quality sleep.
- Talk to your pediatrician – Ask if sleep-disordered breathing might be at play and whether a sleep study would help.
- Seek out an airway evaluation – An airway-focused provider can assess your child’s breathing, jaw development, and sleep patterns.
- Book a consultation with an airway dentist – As someone who works with kids and families on these exact issues every day, I can often spot what others might miss. If you’re local to our Houston or Austin offices—or even if you’re not—we’re happy to help guide you in the right direction.
There’s Hope—and Help
We understand how exhausting and discouraging it can be when nothing seems to work. Many families have tried alarms, medications, and schedules—only to feel stuck in a cycle of frustration and worry.
If your child is still wetting the bed despite traditional treatments, it may be time to consider sleep-disordered breathing as a possible root cause. At The Airway Dentists, our comprehensive evaluations are designed to identify airway-related issues that could be affecting more than just bedwetting. From behavior and mood to focus and development, poor sleep can impact every part of a child’s well-being.
We’re parents, too—and we believe every child deserves to breathe easily, sleep soundly, and wake up dry, confident, and thriving.
FAQs
Can sleep apnea cause bedwetting in adults?
Yes. While this article focuses on children, the same mechanism applies to adults. Sleep apnea disrupts oxygen levels during sleep, which can trigger the body to release urine. In some cases, untreated sleep apnea may contribute to nighttime accidents in adults.
Can sleep apnea cause bedwetting in kids?
Absolutely. Research shows that children with sleep-disordered breathing, including mild sleep apnea, are much more likely to wet the bed. When breathing is disrupted, oxygen levels drop, and the brain triggers a stress response that can override bladder control. Treating airway issues often leads to dry nights within weeks.
Does mouth breathing cause bedwetting?
Yes, mouth breathing at night can be linked to bedwetting. It often signals sleep-disordered breathing, which disrupts oxygen flow and sleep quality. This chain reaction can affect bladder control. Addressing mouth breathing through airway-focused care can improve both sleep and nighttime dryness.
Ready to explore what might be missing?
Let’s find the root cause.
Clinical Research & Supporting Studies:
- Bed-wetting. Mayo Clinic, 2023.
- Nocturnal Enuresis: The Management of Bedwetting in Children and Young People. National Library of Medicine, National Clinical Guideline Centre, 2010.
- Enuresis. National Library of Medicine, 2024.
- The association between obstructive sleep apnea and nocturnal enuresis in children: current advances and research trends. World Journal of Urology, 2025.
- Enuresis in children with sleep apnea. The Journal of Pediatrics, 2003.